Obstructive sleep apnea-hypopnea syndrome (OSAHS) involves repetitive collapse of the upper airway during sleep, leading to reduced or paused breathing.
These respiratory events disrupt normal sleep architecture and decrease oxygen levels. Effective treatment is important for managing symptoms and mitigating increased risks for hypertension, heart disease, diabetes, and stroke.
This article provides an overview of the main therapies used for obstructive sleep apnea-hypopnea.
Positive Airway Pressure Devices
Positive airway pressure (PAP) devices deliver pressurized airflow through a fitted interface such as a mask to structurally splint the airway open throughout sleep. This counters airway collapse that drives obstructive apneic/hypopneic events in OSAHS patients.
Continuous Positive Airway Pressure (CPAP)
Continuous positive airway pressure (CPAP) devices deliver a constant level of pressurized air through a nasal mask to pneumatically splint the airway open.
This prevents airway collapse that causes apneas, hypopneas, and decreased oxygen levels. The pressure is titrated to each patient’s needs based on disease severity.
Common Interface Types Used With CPAP Therapy

CPAP remains the gold standard first-line treatment for moderate to severe OSAHS. It can eliminate respiratory events in most patients and significantly reduce daytime sleepiness when used properly.
However, effectiveness depends on patient adherence in utilizing CPAP therapy every night. Newer auto-adjusting devices like AutoCPAP and SmartCPAP modulate pressure based on sensors detecting airflow.
Bi-Level Positive Airway Pressure (BiPAP)
While CPAP utilizes a single fixed pressure level throughout the respiratory cycle, BiPAP utilizes a more complex dual-level mode of ventilatory support.
BiPAP devices independently monitor inspiratory and expiratory phases of breathing to deliver separate higher inspiratory and lower expiratory pressure levels. This mimics the body’s natural breathing pattern more closely.
During inhalation, a higher pressure is applied to assist inward airflow and ensure adequate ventilation. This higher inspiratory pressure works to splint the airway open and prevent collapse.
On exhalation, automatic sensors cause pressure to rapidly reduce to a lower, more comfortable level. This lower expiratory pressure makes breathing out against the airflow easier and lessen feelings of breathlessness or air trapping.
For patients who struggle to exhale against the constant elevated pressure of CPAP, BiPAP offers a clinically valuable alternative. Its greater pressure variant ability enhances tolerability for those unable to adapt to standard fixed-pressure therapy.
Precisely programmed pressure increase and decreases occur seamlessly breath-by-breath. Multiple ventilation modes further allow customizing to individual patient respiratory characteristics and needs.
With proper titration and support, BiPAP can effectively treat both obstructive and central disordered breathing events while improving comfort over traditional CPAP. It expands therapy options for the sizeable subset of individuals poorly responsive to initial CPAP treatment.
Adaptive Servo Ventilation (ASV)
Some OSAHS patients experience central sleep apnea (CSA) or complex sleep apnea involving both obstructive and central events. ASV devices are specifically tailored for this patient subgroup.
Rather than a fixed continuous airway pressure like CPAP, ASV implements a sophisticated closed-loop servo-controlled system. Embedded sensors and software allow breath-by-breath monitoring of respiratory effort, airflow, and related physiological signals.
Upon detecting respiratory instability or apneic/hypopneic events, the ASV servo-controller rapidly adjusts pressure support levels via its oxygen- and flow-sensing capabilities. It delivers precisely calibrated inspiratory and expiratory pressures that actively stabilize breathing throughout each sleep cycle.
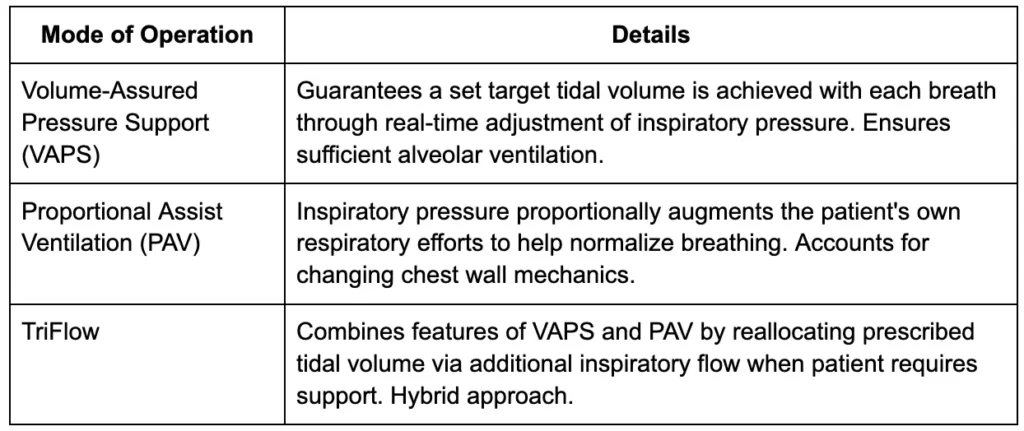
Three Primary Modes of Operation for ASV
Volume-Assured Pressure Support, Proportional Assist Ventilation and TriFlow – address differing extents of respiratory drive and chest-wall compliance. Pressure is dynamically modulated on a breath-to-breath basis within flexible bi-level pressure ranges tailored for each individual.
By responding instantly to disturbances in ventilation, ASV aims to prevent respiratory pauses or insufficient breathing effort that trigger central apneas/hypopneas. It also addresses issue of variable pressure needs during sleep stage transitions and body position changes.
For patients demonstrating significant central/mixed pathology, ASV offers superior treatment of their complex underlying sleep disordered breathing physiology compared to fixed-pressure therapies alone. Careful titration and clinical follow-up are nonetheless important with ASV therapy.
NightLase®
Through a novel application of controlled light energy, NightLase® seeks to gently condition key oral tissues over multiple sessions. Specific structures within the mouth such as the soft palate and tongue are targeted for a natural collagen-induced strengthening.
This delicate tightening effect is designed to reduce unnecessary vibration during rest, lowering disruptions from snoring or other breathing irregularities. As a non-invasive approach, NightLase® does not require anesthesia and aims to minimize discomfort. Multiple practitioners have successfully integrated this therapy into their routines.
The standardized protocol involves three to five laser treatments over approximately six to ten weeks. Initial outcomes seem encouraging and may endure for up to one year, allowing time for reprieve or readjustment as needed.
Oral Appliance Therapy
Oral appliances are another effective treatment option, especially for mild to moderate OSAHS patients. These devices help maintain an open airway by advancing the lower jaw or tongue.
Mandibular Advancement Devices
Custom-made mandibular advancement devices (MADs) fit similar to a mouth guard and are adjusted to shift the lower jaw slightly forward during sleep. This prevents the tongue from collapsing backward and obstructing airflow. MADs are an alternative for patients who cannot tolerate CPAP therapy.
Tongue-Retaining Devices
These appliances have a suction bulb that holds the tongue forward to prevent it from obstructing the airway. They may be indicated for patients with tongue base obstruction.
Oral appliances are non-invasive and convenient but require custom fitting and adjustment. They are generally not as effective as CPAP for more severe OSAHS. Side effects can include tooth discomfort, excessive salivation, and jaw pain.
Surgical Treatment Options
Various surgical techniques alter the anatomy to increase airway caliber and prevent collapse that contributes to OSAHS. Surgery may be considered for moderate to severe cases that do not respond adequately to other therapies.
Palatal Surgery
The palate is a primary site of collapse, so procedures aim to remodel and stiffen this area. As shown in the table below, uvulopalatopharyngoplasty (UPPP) trims excess palate and uvula tissue via an oral procedure.
Laser-assisted uvulopalatopharyngoplasty uses laser energy for the same effect in an office setting. Palatal implants insert stabilizing material under the soft palate. However, palate surgery alone provides limited success due to frequency of tongue base involvement.

Tongue Base Surgery
Obstruction frequently occurs where the tongue meets the pharynx (glosso-epiglottic level).
Advancing the genioglossus muscles via genioglossus advancement or pulling mandible/hyoid forward with hyoid suspension procedures aim to decrease this. Radiofrequency ablation uses heat energy to shrink and stiffen excess tissue in the oropharynx.
Maxillomandibular Advancement
This more extensive orthognathic surgery moves the entire maxilla and mandible forward, increasing retropharyngeal space beyond the tongue root.
It addresses multi-level collapse but complexity requires maxillofacial surgical expertise and significant recovery.
Multi-Level Surgery
Given OSAHS often involves multiple sites, combining approaches that target the palate, tongue base and mandible may offer superior outcomes over single procedures.
However, longer operating times under general anesthesia also increase risks. Careful patient evaluation is key to selecting the optimal surgical strategy.
Additional Treatment Strategies
Additional treatment strategies aim to impact underlying OSAHS pathology through non-device modalities:
Positional Therapy
Since OSAHS is often worse in the supine position, positional therapy aims to prevent sleeping on the back. This approach includes specialized pillows, alarms, and wearable devices. It can be beneficial for mild positional OSAHS.
Weight Loss
Losing weight reduces fatty tissue deposits around airway structures that contribute to their tendency to collapse during sleep. For overweight OSAHS patients, weight reduction through diet, exercise and bariatric surgery can improve sleep apnea severity.
Inspiratory Muscle Training
Strengthening the inspiratory muscles using resistive exercises may help compensate for weakened dilator muscles that aggravate airway collapse. This therapy remains investigational but could supplement other primary OSAHS treatments.
Hypoglossal Nerve Stimulation
An implantable device using a stimulation lead attached to the hypoglossal nerve activates key tongue muscles to maintain airway patency during sleep. It may benefit select OSAHS patients intolerant of CPAP who have obstruction at the tongue base.
Combination and Adjunctive Therapies
Using positive airway pressure along with an oral appliance or upper airway surgery may provide additive benefits in controlling OSAHS. Adjunctive strategies like positional therapy and weight loss can also optimize first-line treatments. Developing individualized, multi-modal care plans helps improve adherence and outcomes.
Conclusion – Personalized Management for OSAHS
CPAP, oral appliances, and surgical modifications of the upper airway are the cornerstones of therapy for obstructive sleep apnea-hypopnea. Newer modalities like hypoglossal nerve stimulation continue to emerge as additional options.
Devising tailored treatment regimens based on each patient’s anatomy, disease severity, tolerance, and adherence helps optimize real-world efficacy.
Ongoing advances in OSAHS management aim to improve quality of sleep and health.