Do you struggle to fall asleep or stay asleep throughout the night? Do little sounds or movements that go unnoticed by others keep you wide awake? If this sounds familiar, you may have sensory processing disorder (SPD).
At Allure Medical, we know that living with SPD presents daily challenges. One major area affected is often sleep. For those with SPD, sensory hypersensitivities frequently disrupt falling and staying asleep. The result is tossing, turning and restless nights.
What is Sensory Processing Disorder?
Sensory processing disorder refers to the way your brain processes sensations and stimuli from your environment. Your senses include sight, sound, taste, smell, touch, balance and movement. Typically, the brain can take in sensory information, organize it, and respond appropriately.
With SPD, the central nervous system has difficulty handling sensory signals. You may be oversensitive to some inputs and undersensitive to others. Or your brain may struggle to process multiple sensory inputs at once. This makes it hard to execute ordinary daily tasks and interact with the world effectively.
SPD can affect one or more senses:
- Auditory processing disorder – difficulty interpreting sounds
- Visual processing disorder – trouble interpreting visual information
- Tactile sensory disorder – oversensitivity to touch
- Olfactory processing disorder – increased sensitivity to smells
- Gustatory processing disorder – hypersensitivity to tastes
- Vestibular sensory disorder – problems with balance and spatial orientation
- Proprioceptive sensory disorder – difficulty sensing body movements and position
What Are the Main Types of Sensory Processing Disorder?
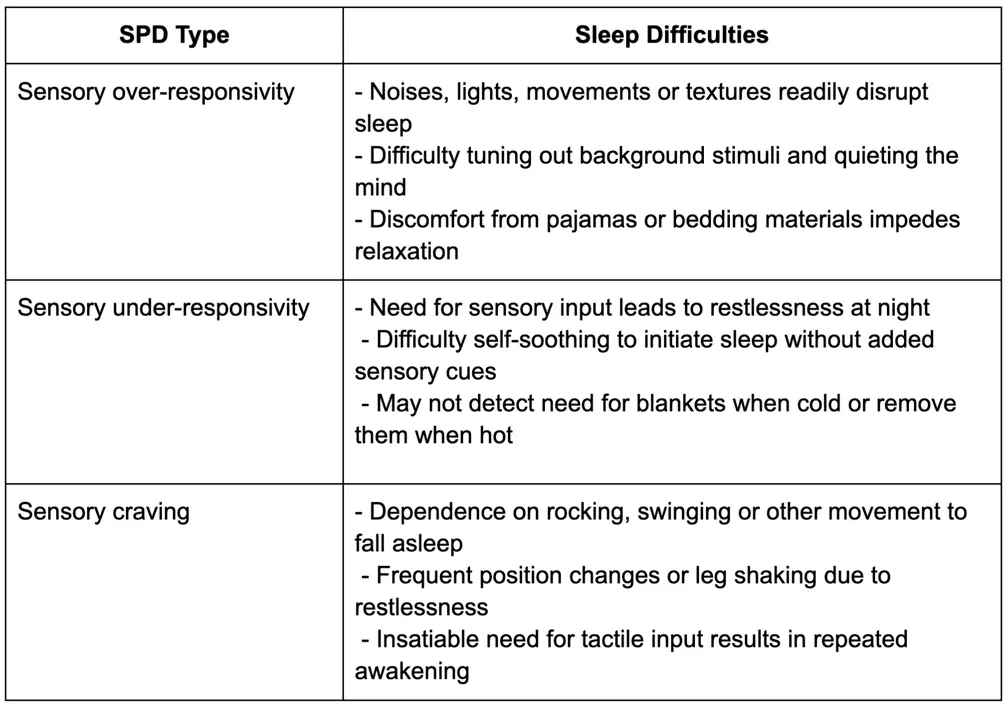
There are three main types of SPD that reflect how the brain responds to sensory stimuli:
- Sensory over-responsivity: You have a stronger response to a sensory input than most people. Sights, textures, tastes or other stimuli are experienced as intolerable or even painful. For example, certain clothing fabrics may cause extreme discomfort.
- Sensory under-responsivity: You have a lower sensitivity than normal to sensory cues. You may not notice or respond to stimuli that others clearly perceive. For instance, you may seem unaware of loud sounds or temperatures that typically evoke reactions.
- Sensory craving: You actively seek out sensory experiences such as movement, touch, sound or other intense stimuli. You have almost an insatiable need for sensory input. This often manifests in “sensory seeking” behaviors.
What Is the Difference Between Sensory Integration Disorder and Sensory Processing Disorder?
In the past, sensory processing issues were referred to as sensory integration dysfunction or disorder. Today, most medical professionals use the umbrella term sensory processing disorder.
Sensory integration disorder specifically described challenges with taking in and making sense of sensory information. Sensory processing disorder has a broader meaning. SPD encompasses sensory modulation issues like over-responsiveness and under-responsiveness. It also includes sensory discrimination challenges and sensory-based motor disorders.
So in short – all sensory integration disorder is sensory processing disorder. But not all sensory processing disorders are strictly sensory integration issues. SPD better captures the diverse range of sensory difficulties individuals can experience.
What Is Currently Understood About the Causes of Sensory Processing Disorder?
Researchers are still working to uncover the exact causes of SPD. However, they suspect that it stems from the brain and nervous system not processing sensory signals typically during critical developmental periods.
Contributing factors may include:
- Genetics – SPD appears to run in families, suggesting a hereditary component.
- Low birth weight, prematurity or birth trauma – This can disrupt normal sensory pathway development.
- Neurological differences – Developmental disorders like autism often coincide with sensory modulation issues.
- Brain structure – Some studies reveal subtle brain anatomy variations in SPD patients.
While the precise origins require more research, SPD seems to arise from biological predispositions combined with environmental conditions during early development. The good news is that treatment and therapy can help regardless of the cause.
How Does Sensory Processing Disorder Impact Sleep?
For those with SPD, sensory challenges and sleep problems often go hand-in-hand.
Sensory hypersensitivities make it hard to block out trivial stimuli that prevent falling asleep. And research indicates that insufficient sleep diminishes the brain’s capacity to process sensory input effectively during the day.
Let’s look at how different types of SPD can interfere with getting adequate rest:
Whatever your specific sensitivities, the inability to stop processing sensory information strains quality slumber.
What are the Signs That SPD is Affecting Your Sleep?
You may wonder if SPD is solely a childhood condition that eases with maturity. But for many, sensory regulation problems persist throughout adulthood.
So if you are an adult who continues battling sensory challenges, you likely understand how this affects your bedtime routine and sleep patterns. You may:
- Lie awake listening to a partner’s breathing, snoring or slight movements
- Be hyperaware of ambient sounds like fans, alarms or pets stirring
- Toss and turn trying to find a comfortable sleeping position
- Frequently adjust blankets and pillows attempting to feel “just right”
- Remove restrictive pajamas or irritating socks while sleeping
- Need to get up for snacks, drinks or sensory motions to enable falling back asleep
- Feel exhausted upon waking despite long sleep durations
Adult sensory issues may also contribute to heightened anxiety and worry at bedtime. And sleep deprivation often worsens over-responsiveness. So without solutions, you may become stuck in an endless sleepless cycle.
If you see yourself in these sleep struggle patterns, know there are solutions available. One option to consider is NightLase® laser treatment.
Strategies to Improve Sleep with Sensory Processing Disorder
Since sensory regulation and sleep are so intertwined, tailored interventions can improve sleep for those with SPD. Strategies may include:
- Setting up a soothing bedtime routine – Unwind with calm activities away from stimuli.
- Making the bedroom a sensory refuge – Use blackout curtains, white noise, and comfortable, breathable bedding.
- Addressing underlying issues – Treat coexisting sleep disorders or health conditions contributing to sensory problems.
- Occupational therapy – Collaborate with an OT to identify sensory accommodations and routines.
- Cognitive behavioral therapy – A CBT therapist provides tools to shift sleep-disrupting thought patterns.
NightLase® for Improved Sleep with Sensory Processing Disorder
For those with sensory processing disorder (SPD), sleep struggles are common. Sensory hypersensitivities make it hard to tune out trivial noises, lights, textures, and movements that disrupt sleep.
NightLase® treatment may help in two key ways:
- By tightening and strengthening throat tissues, NightLase can reduce snoring and sleep apnea. This eliminates those noises that can keep SPD patients awake.
- By improving sleep quality and duration, NightLase enables better sensory processing during the day. Research shows that adequate sleep enhances the brain’s ability to regulate sensory input.
NightLase® offers a drug-free and non-invasive way to improve sleep for those with SPD. Consult your provider to see if it may be an appropriate option to resolve your sleep difficulties. More restful nights can in turn improve sensory regulation during waking hours.
Don’t wait – contact Allure Medical today to start resolving your sleep challenges once and for all.